Differences Between Rheumatoid Arthritis and Osteoarthritis
What Is The Difference Between Osteoarthritis And Rheumatoid Arthritis?
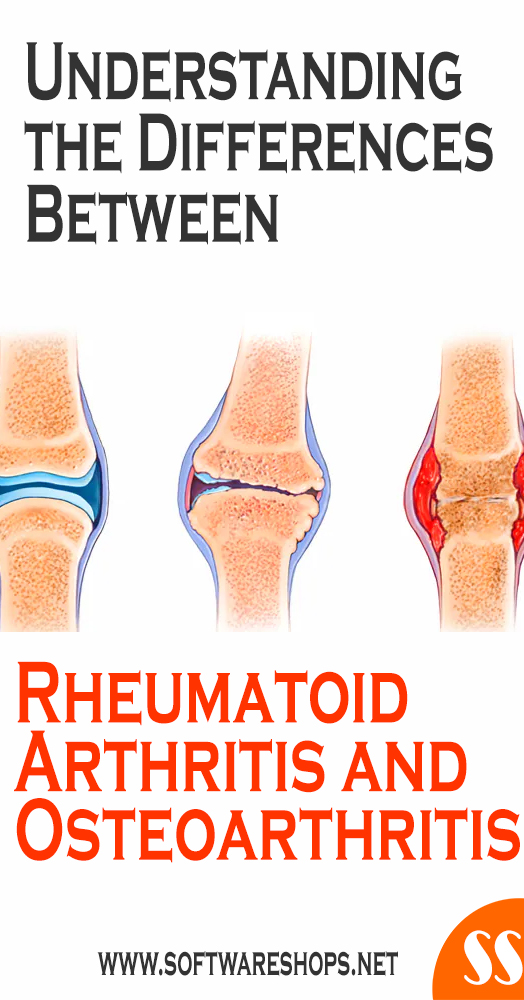
Rheumatoid arthritis and osteoarthritis are two different diseases, despite two “sound” very similar and both affecting the joints causing joint problems. Let’s see the differences between them.
It is logical that rheumatoid arthritis and osteoarthritis are confused, that is why in this article we will review the differences between these two disorders.
The term “arthritis” is used a lot as if it was a single condition, but the word can refer to many different types of conditions that involve joint pain. One is degenerative – osteoarthritis (OA) – and the other is an autoimmune condition – rheumatoid arthritis (RA).
Broadly speaking, rheumatoid arthritis is a curable disease caused by an inflammatory process in the joint, while osteoarthritis is an irreversible disease caused by the wear and tear of cartilage.
These two rheumatological diseases cause pain in the areas of the body where they develop. Knowing the differences is important, as effective and rapid detection can be vital to prevent or slow its progression.
There are similarities between the two conditions. For example, both cause chronic joint pain, and both are more common in women. But they have different causes, symptoms, treatments, and prognoses. Find out more about how to differentiate them.
Rheumatoid Arthritis And Osteoarthritis: What Differentiates Them?
Rheumatoid arthritis and osteoarthritis are two of the most common rheumatic diseases. Both disorders have in common that they occur with pain and that they are more frequent in women. However, there are many other ways in which they differ.
Here are these differences.
1. Damaged Tissue
The main difference between rheumatoid arthritis and osteoarthritis (and from which all the others derive) is the tissue that is affected:
Rheumatoid Arthritis:
Rheumatoid Arthritis is a disease in which inflammation of the joints occurs due to excess synovial fluid. In it, the synovial membrane is damaged, a structure that is responsible for producing synovial fluid, which works as a lubricant in the joints to allow proper movement.
Under normal conditions, this synovial fluid is being reabsorbed. However, with the development of this disease, it spreads through the joint, causing the bone and cartilage to constantly rub against each other. This leads to an erosion of these two structures, which causes pain.
Osteoarthritis:
Osteoarthritis is a disease characterized by the degeneration of cartilage. Cartilages are structures found in the joints and that are located between the bones, functioning as a kind of pad that prevents these bones from rubbing against each other.
With osteoarthritis, these cartilages in the joints wear out in a chronic degenerative process that ends up assuming their loss. Not having cartilage means that the bones erode one another, which causes pain and loss of mobility of the joints.
2. Causes
The origin of these two diseases is also different.
Rheumatoid Arthritis:
Rheumatoid Arthritis is a disease that can have different causes. The most common of these is an autoimmune disorder in which the body attacks certain cells by mistake, thus damaging the synovium and causing excess inflammatory fluid. Although it continues to be studied, this appears to be the most common cause.
Rheumatoid Arthritis can also be due to an infection, as there are certain pathogens (bacteria and viruses) that are capable of reaching the joints and reproducing in them. This causes the cells of the immune system to move to them and start the inflammatory process, which in this case is a response to an external threat.
Another cause of rheumatoid arthritis is trauma, as a severe contusion to the joints can cause injuries in which synovial fluid spreads through the joint. This also explains the inflammation and pain with which the disease occurs.
Osteoarthritis:
Osteoarthritis is a chronic degenerative process, so it does not have the same causes as arthritis. Osteoarthritis is usually simply related to aging since cartilage wear over the years can end up causing it to be lost, giving rise to this pathology.
However, it is true that there are some risk factors such as obesity because the cartilage must support more weight than normal, it wears out more easily. Another risk factor is being an elite athlete or any other person with a job in which there is continuous overstressing of the joints.
3. Affected Population and Frequency
These two diseases do not affect the same people nor do they occur with the same frequency in the population.
Rheumatoid Arthritis:
The main characteristic of rheumatoid arthritis is that it can affect anyone regardless of gender or age. Although it is usually more common in women between 30 and 50 years old, as it is an autoimmune disease or of infectious origin, its incidence is not understood by population groups.
Also, rheumatoid arthritis is less common than osteoarthritis. It is estimated that it affects between 0.3% and 1% of the world population, which means that in the world there are between 100 and 200 million people affected by this disorder. Both conditions are more common in women; 75% of people with rheumatoid arthritis are women.
Osteoarthritis:
Osteoarthritis are the most common forms of arthritis, about 10 times more common than rheumatoid arthritis. Osteoarthritis affects an estimated 27 million Americans, while rheumatoid arthritis affects 1.3 million.
Osteoarthritis, on the other hand, being due to a degenerative process of the cartilage, affects more the elderly population, especially women. It usually shows symptoms from the age of 40, although these gradually worsen as age increases.
Osteoarthritis is much more common than arthritis. In fact, almost 50% of the population develops osteoarthritis to a greater or lesser degree. After the age of 80, almost all people have signs of suffering from osteoarthritis, since it is almost inevitable that throughout life there has been no wear of the cartilage.
4. Symptoms
Symptoms also vary depending on the disease. Although both are characterized by joint pain and joint stiffness, especially in the morning, there are some differences to take into account:
Rheumatoid Arthritis:
The main sign of rheumatoid arthritis is that the pain in the joint is greater during rest, although movement is also observed. Joint stiffness appears upon waking, and it can take up to an hour to regain proper mobility.
Rheumatoid arthritis is usually a general discomfort, although it is felt more in the joints with more movement, especially hands, feet, knees, wrists, elbows…
In addition to this pain that intensifies with rest, there is heat, redness, and swelling in the joint. All these symptoms are due to inflammation caused by excess synovial fluid.
It can be linked to other symptoms: tiredness, fever (if there is an infection), dry mouth, hoarseness, tingling in the extremities, etc.
Osteoarthritis:
In osteoarthritis, unlike arthritis, the pain is greater during movement. Morning joint stiffness does not take an hour to go away, but usually within a few minutes. Although rheumatoid arthritis was when there was more pain, being at rest is a relief for those affected by this disease, since there is no friction between the bones and therefore there is no pain.
Osteoarthritis is not a general discomfort like rheumatoid arthritis was, but rather it is characterized by localized pain at a very specific point. Arthrosis of the hands are the most common osteoarthritis, as it has the most susceptible joints to be worn out, although osteoarthritis of the knees, feet, and hips is also typical.
In osteoarthritis, as there is no inflammatory process, there is no heat release from the joint or redness. However, you may notice some numbness and even swelling.
CLICK TO READ: Most Effective Ways To Overcome Knee Pain Relief At Home
5. Diagnosis
Detecting the presence of these two diseases early is essential to start the appropriate treatments.
Rheumatoid Arthritis:
In the case of arthritis, the rheumatologist will observe the type of inflammation that the patient suffers. To confirm that you have developed arthritis, blood or synovial fluid tests are performed to see the presence of autoimmune disorders or infective processes.
Osteoarthritis:
On the other hand, in osteoarthritis, as it is a simply degenerative process, it would not be useful to perform blood or synovial fluid tests, since no abnormality would be observed.
Osteoarthritis is diagnosed by a mere physical examination and analysis of symptoms. The clinical picture is the most important part of the detection, since taking X-rays is not always useful, since there are times when there is osteoarthritis and the X-rays come out well. Or vice versa, since X-rays seem to indicate signs of osteoarthritis but the person does not have any symptoms.
6. Treatment
Once one of the two diseases are detected, the corresponding treatment is started:
Rheumatoid Arthritis:
Rheumatoid Arthritis is treated with anti-inflammatory drugs, as they are designed to reduce excess inflammation to alleviate symptoms. In addition to resting the joint to reduce excess synovial fluid, it can be treated with antibiotics if the origin of the disorder is an infection. Ultimately, rheumatoid arthritis is a disease that with proper treatment is curable.
Osteoarthritis:
On the other hand, osteoarthritis is a disease for which there is no cure since cartilage wear is irreversible. Therefore, it becomes a chronic disorder with a treatment based on preventing the degeneration from going further.
For those with mild osteoarthritis symptoms, several lifestyle changes are recommended to help manage symptoms. These include:
- If overweight, losing weight
- Wearing proper footwear
- Exercise regularly
Using devices that help reduce the amount of deformation placed on the joints daily
The therapy is focused on using medications that reduce pain (analgesics) and improve joint mobility. It is also advisable to avoid being overweight and doing physical activity, as long as it does not force the affected joint.
If you’re experiencing joint pain, don’t self-diagnose or just assume that you have arthritis. Make an appointment with your primary care doctor to discuss your symptoms. If necessary, your primary care physician will refer you to a rheumatologist, a doctor who specializes in musculoskeletal and autoimmune diseases.
With a proactive approach to lifestyle, making appropriate changes in the way things are done, and keeping physically active, with medications as prescribed during regular check-ups, osteoarthritis patients can experience significant relief in pain and mood.